Metacarpal phalangeal fractures are common fractures in hand trauma, accounting for about 1/4 of hand trauma patients. Due to the delicate and complex structure of the hand and the delicate function of movement, the importance and technicality of hand fracture treatment are far more complex than the treatment of other long bone fractures. Ensuring the stability of the fracture after reduction is the key to the successful treatment of metacarpal phalangeal fractures. In order to restore the function of the hand, fractures often require appropriate fixation. In the past, plaster external fixation or Kirschner wire internal fixation was often used, but it is often not conducive to early postoperative joint rehabilitation training due to inaccurate fixation or long fixation time, which has a greater impact on the recovery of finger joint function and brings certain difficulties to the functional rehabilitation of the hand. Modern treatment methods are increasingly using stronger internal fixation, such as micro-plate screw fixation.
I. What are the treatment principles?
The treatment principles for hand metacarpal and phalangeal fractures: anatomical reduction, light and firm fixation, early activities and functional training. The treatment principles for intra-articular and peri-articular fractures of the hand are the same as those for other intra-articular fractures, which are also to restore the anatomy of the joint surface and early functional activities. When treating hand metacarpal and phalangeal fractures, efforts should be made to achieve anatomical reduction, and rotation, lateral angulation, or angular displacement of >10° to the dorsal aspect of the palm should not occur. If the fracture end of the metacarpal phalange rotates or angularly displaces laterally, it will change the trajectory of the normal flexion and extension movement of the finger, causing it to shift or fall with the adjacent finger during flexion, affecting the accuracy of the finger function; and when the angular displacement to the dorsal aspect of the palm is >10°, the smooth contact surface between the bone and the tendon is destroyed, increasing the resistance and range of motion of the flexion and extension of the tendon, and chronic tendon damage occurs, inducing the risk of tendon rupture.
II. What materials can be selected for metacarpal fractures?
There are many internal fixation materials for metacarpal fractures, such as Kirschner wires, screws, plates and external fixators, among which Kirschner wires and microplates are the most commonly used. For metacarpal fractures, microplate internal fixation has obvious advantages over Kirschner wire fixation and can be used first; for proximal phalanx fractures, microplates are generally superior, but when it is difficult to insert screws for proximal phalanx distal segment and head fractures, cross Kirschner wire internal fixation should be used, which is more conducive to the recovery of the function of the affected finger; Kirschner wires should be used first for the treatment of middle phalanx fractures.
- Kirschner wire: Kirschner wire internal fixation has been used in clinical practice for more than 70 years and has always been the most commonly used internal fixation material for metacarpal and phalangeal fractures. It is easy to operate, economical and practical, and is the most classic internal fixation method. As the most commonly used internal fixation for the treatment of hand fractures, it is still widely used. Advantages of Kirschner wire internal fixation: ① Easy to operate and very flexible to use; ② Less soft tissue stripping, less impact on the blood supply of the fracture end, less surgical trauma, and conducive to fracture healing; ③ Easy to remove the needle for the second time; ④ Low cost and wide range of application, suitable for most hand fractures (such as intra-articular fractures, severe comminuted fractures and distal phalangeal fractures).


2.Metacarpophalangeal microplates: Strong internal fixation of hand fractures is the basis for early functional training and a necessary condition for restoring good hand function. AO internal fixation technology requires that the fracture ends be precisely repositioned according to the anatomical structure and that the fracture ends be stable under functional conditions, which is commonly known as strong fixation, in order to allow early active movement. AO also emphasizes minimally invasive surgical operations, with the focus on protecting blood supply. Microplate internal fixation for the treatment of hand fractures can achieve satisfactory results in terms of strength, stability of fracture ends, and pressure between fracture ends. In terms of postoperative functional recovery, fracture healing time, and infection rate, it is believed that the efficacy of microtitanium plates is significantly better than that of Kirschner wires. Moreover, since the fracture healing time after fixation with microtitanium plates is significantly shorter than that of other fixation methods, it is beneficial for patients to resume normal life early.


(1) What are the advantages of microplate internal fixation?
① Compared with Kirschner wires, microplate screw materials have better tissue compatibility and better tissue response; ② The stability of the plate-screw fixation system and the pressure on the fracture end make the fracture closer to anatomical reduction, more secure fixation, and conducive to fracture healing; ③ Early functional exercise is generally allowed after microplate fixation, which is conducive to the recovery of hand function.
(2)What is the surgical method for microplates?
The surgery is usually performed under brachial plexus block anesthesia, and a pneumatic tourniquet is usually required. The dorsal incision of the metacarpal phalanges is taken, the dorsal aponeurosis of the digits is cut or the interosseous muscle and metacarpal bone are entered to expose the fracture ends of the metacarpal or phalangeal bones, the periosteum is peeled off, and the fracture is reduced under direct vision. Straight plates are suitable for transverse fractures of the middle segment and short oblique fractures, T-plates are suitable for fixation of the base of the metacarpal and phalanges, and T-plates or 120° and 150° L-plates are suitable for fixation of long oblique and comminuted fractures. The plate is generally placed on the dorsal side of the bone to prevent tendon sliding and long-term wear, which is conducive to early functional training. At least two screws should be used to fix the two ends of the fracture, otherwise the stability is poor, and Kirschner wires or screws outside the plate are needed to assist fixation to achieve the purpose of stable fixation.


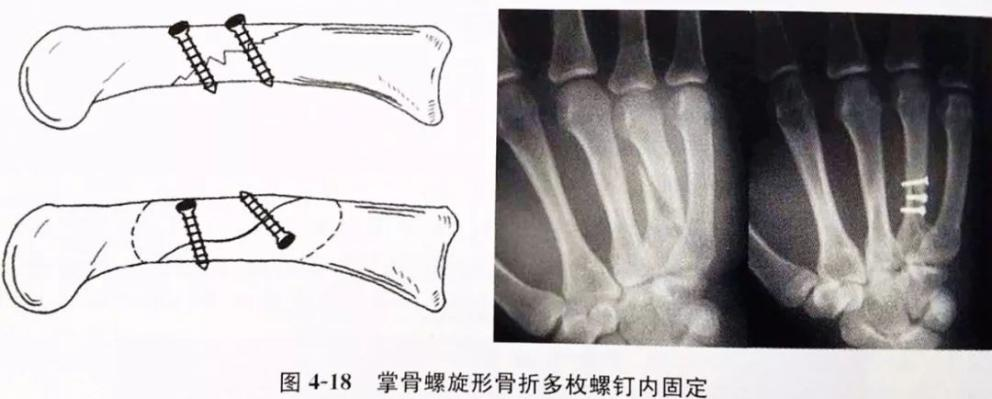
3.Mini screws: Mini screws have similar stability to steel plates in the fixation of spiral or long oblique fractures, but the range of soft tissue and periosteum stripping is smaller than that of steel plate fixation, which is conducive to protecting blood supply and in line with the concept of minimally invasive operation. Although there are T-type and L-type plates for near-articular fractures, the recovery of joint function after postoperative follow-up is worse than that of diaphyseal fractures. Mini screws also have certain advantages in the fixation of intra-articular and peri-articular fractures. The screws screwed into the cortical bone can withstand a large stress load, so the fixation is firm, and the fracture ends can be compressed to make the fracture surface in close contact, shorten the fracture healing time and facilitate the healing of the fracture, as shown in Figure 4-18. Mini screw internal fixation of hand fractures is mainly used for oblique or spiral fractures of the diaphyseal and intra-articular avulsion fractures of larger bone blocks. It should be noted that when using mini screws alone to fix oblique or spiral fractures of the diaphyseal bone of the hand, the length of the fracture line should be at least twice the diameter of the diaphyseal bone, and when fixing avulsed fracture blocks in the joint, the width of the bone block should be at least 3 times the diameter of the thread.

4.Micro external fixator: Comminuted metacarpal phalangeal fractures are sometimes difficult to anatomically reduce or cannot be firmly fixed internally even after surgical incision due to the destruction of the bone support. The external fixator can restore and maintain the length of the comminuted fracture under traction, playing a role of relative fixation. Different metacarpal phalangeal external fixators are placed in different positions: the 1st and 2nd metacarpal phalanges are placed on the dorsal radial side, the 4th and 5th metacarpal phalanges are placed on the dorsal ulnar side, and the 3rd metacarpal phalange is placed on the dorsal radial side or dorsal ulnar side according to the situation. Pay attention to the needle insertion point to prevent tendon damage. Closed fractures can be reduced under X-rays. When the reduction is not ideal, a small incision can be performed to assist in reduction.
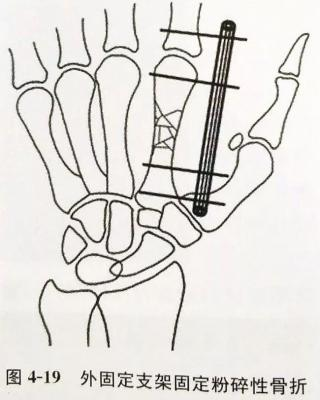


What are the advantages of external fixators?
① Simple operation, can adjust various displacements of fracture ends; ② Can effectively reduce and fix intra-articular fractures of metacarpophalangeal bones without damaging the joint surface, and can distract the joint surface to prevent contracture of joint capsule and collateral ligament; ③ When comminuted fractures cannot be anatomically reduced, they can be combined with limited internal fixation, and the external fixator can partially reduce and maintain the force line; ④ Allow early functional exercises of the affected finger in the unfixed joint to avoid joint stiffness and osteoporosis; ⑤ Can effectively fix hand fractures without affecting the postoperative treatment of the wound on the affected hand.
Post time: Dec-21-2024











