Currently for internal fixation of distal radius fractures, there are various anatomical locking plate systems used in the clinic. These internal fixations provide a better solution for some complex fracture types, and in some ways expand the indications for surgery for unstable distal radius fractures, especially those with osteoporosis. Professor Jupiter from Massachusetts General Hospital and others have published a series of articles in JBJS on their findings on locking plate fixation of distal radius fractures and related surgical techniques. This article focuses on the surgical approach to fixation of distal radius fractures based on internal fixation of a specific fracture block.
Surgical Techniques
The three-column theory, based on the biomechanical and anatomical characteristics of the distal ulnar radius, is the basis for the development and clinical application of the 2.4mm plate system. The division of the three columns is shown in Figure 1.

Fig. 1 Three-column theory of the distal ulnar radius.
The lateral column is the lateral half of the distal radius, including the navicular fossa and the radial tuberosity, which supports the carpal bones on the radial side and is the origin of some of the ligaments that stabilise the wrist.
The middle column is the medial half of the distal radius and includes the lunate fossa (associated with the lunate) and sigmoid notch (associated with the distal ulna) on the articular surface. Normally loaded, the load from the lunate fossa is transmitted to the radius via the lunate fossa. The ulnar lateral column, which includes the distal ulna, the triangular fibrocartilage, and the inferior ulnar-radial joint, carries loads from the ulnar carpal bones as well as from the inferior ulnar-radial joint and has a stabilising effect.
The procedure is performed under brachial plexus anaesthesia and intraoperative C-arm X-ray imaging is essential. Intravenous antibiotics were administered at least 30 minutes before the start of the procedure and a pneumatic tourniquet was used to reduce bleeding.
Palmar plate fixation
For most fractures, a palmar approach can be used to visualise between the radial carpal flexor and the radial artery. After identifying and retracting the flexor carpi radialis longus, the deep surface of the pronator teres muscle is visualised and the "L" shaped separation is lifted. In more complex fractures, the brachioradialis tendon may be further released to facilitate fracture reduction.
A Kirschner pin is inserted into the radial carpal joint, which helps to define the distal-most limits of the radius. If a small fracture mass at the articular margin is present, a palmar 2.4mm steel plate can be placed over the distal articular margin of the radius for fixation. In other words, a small fracture mass on the articular surface of the lunate can be supported by a 2.4mm "L" or "T" plate, as shown in Figure 2.

For dorsally displaced extra-articular fractures, it is helpful to note the following points. Firstly, it is important to temporarily reset the fracture to make sure that there is no soft tissue embedded in the fracture end. Secondly, in patients without osteoporosis, the fracture can be reduced with the assistance of a plate: first, a locking screw is placed at the distal end of a palmar anatomical plate, which is secured to the displaced distal fracture segment, then the distal and proximal fracture segments are reduced with the assistance of the plate, and finally, other screws are placed proximally


FIGURE 3 Extra-articular fracture of the dorsally displaced distal radius is reduced and fixed via a palmar approach. FIGURE 3-A After completion of the exposure via the radial carpal flexor and the radial artery, a smooth Kirschner pin is placed into the radial carpal joint. Figure 3-B Manipulation of the displaced metacarpal cortex to reset it.

Figure 3-C and Figure 3-D A smooth Kirschner pin is placed from the radial stem through the fracture line to temporarily fix the fracture end.
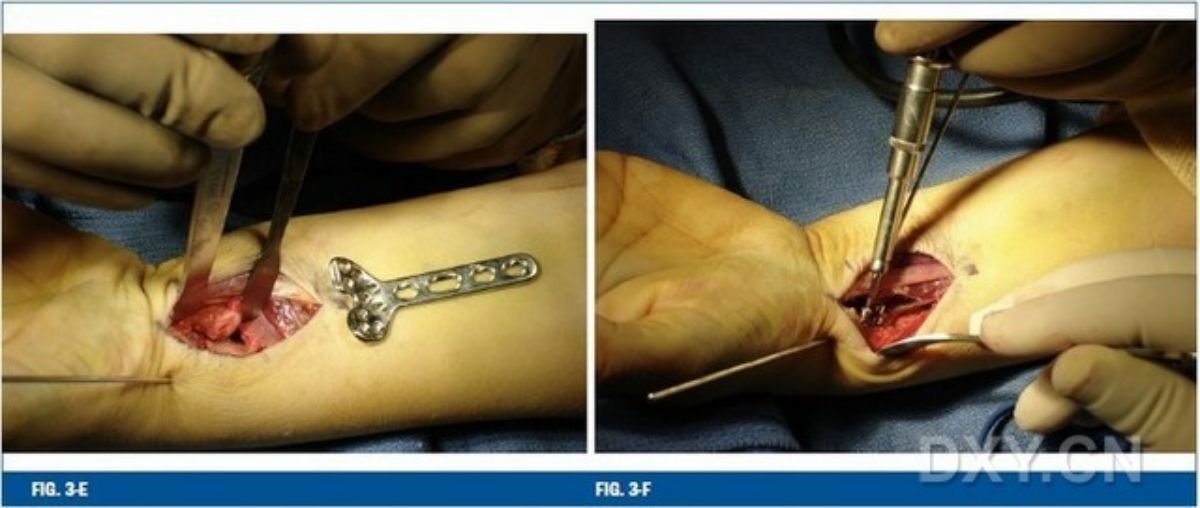
Fig. 3-E Adequate visualisation of the operative field is achieved by using a retractor prior to plate placement. FIGURE 3-F Distal row of locking screws is placed near the subchondral bone at the end of the distal fold.
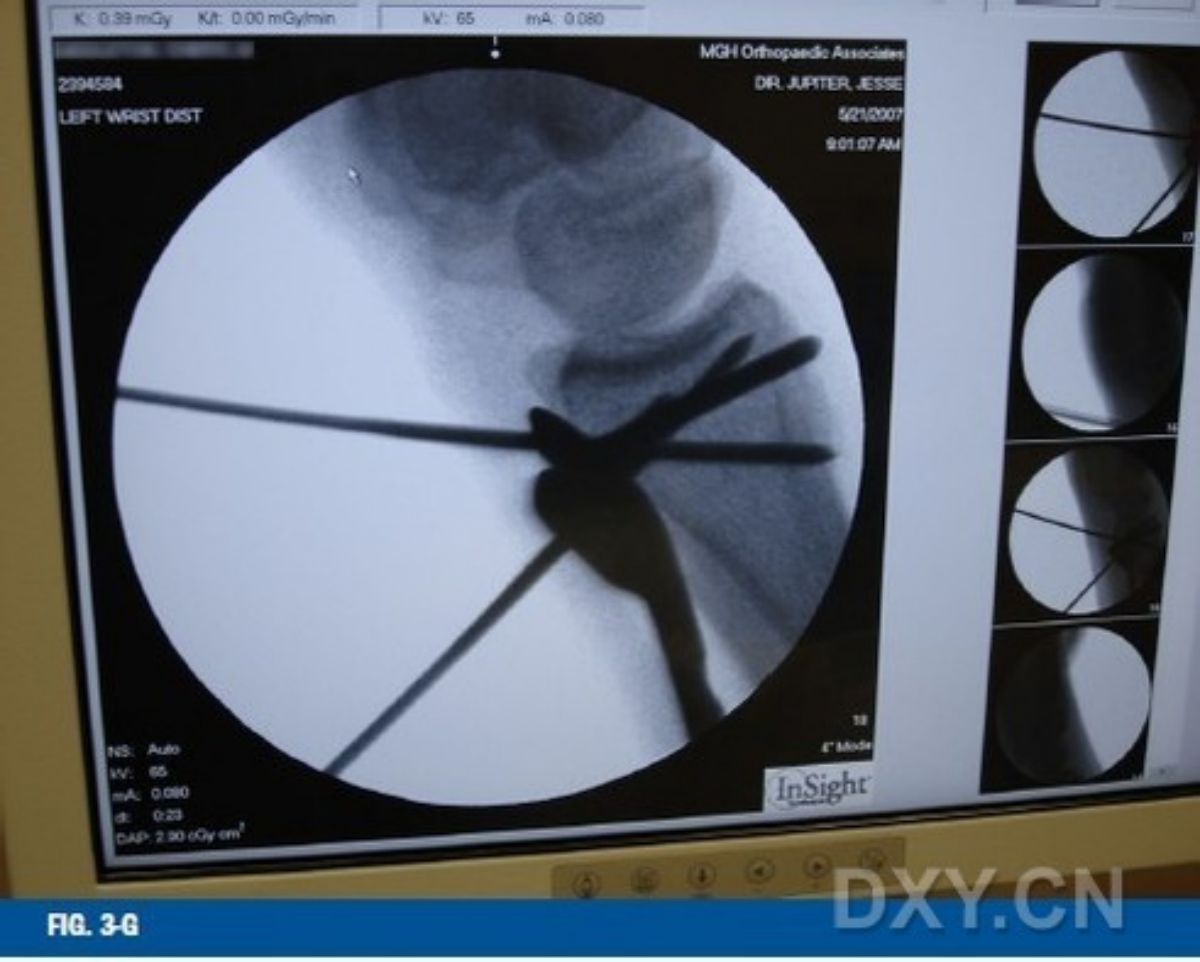


Figure 3-G X-ray fluoroscopy should be used to confirm the position of the plate and distal screws. Figure 3-H The proximal portion of the plate should ideally have some clearance (10 degree angle) from the diaphysis so that the plate can be fixed to the diaphysis to further reset the distal fracture block. Figure 3-I Tighten the proximal screw to reestablish the palmar inclination of the distal fracture. Remove the Kirschner pin before the screw is fully tightened.


Figures 3-J and 3-K Intraoperative radiographic images confirm that the fracture was finally anatomically repositioned and the plate screws were satisfactorily positioned.
Dorsal Plate Fixation The surgical approach to expose the dorsal aspect of the distal radius depends mainly on the type of fracture, and in the case of a fracture with two or more intra-articular fracture fragments, the goal of the treatment is mainly to fix both the radial and the medial columns at the same time. Intraoperatively, the extensor support bands must be incised in two main ways: longitudinally in the 2nd and 3rd extensor compartments, with subperiosteal dissection to the 4th extensor compartment and retraction of the corresponding tendon; or a second support band incision between the 4th and 5th extensor compartments to expose the two columns separately (Fig. 4).
The fracture is manipulated and temporarily fixed with an unthreaded Kirschner pin, and radiographic images are taken to determine that the fracture is well-displaced. Next, the dorsal ulnar (middle column) side of the radius is stabilised with a 2.4 mm "L" or "T" plate. The dorsal ulnar plate is shaped to ensure a tight fit on the dorsal ulnar side of the distal radius. The plates can also be placed as close to the dorsal aspect of the distal lunate as possible, as the corresponding grooves on the underside of each plate allow the plates to be bent and shaped without damaging the threads in the screw holes (Fig. 5).
Fixation of the radial column plate is relatively simple, as the bone surface between the first and second extensor compartments is relatively flat and can be fixed in this position with a properly shaped plate. If the Kirschner pin is placed in the extreme distal part of the radial tuberosity, the distal end of the radial column plate has a groove that corresponds to the Kirschner pin, which does not interfere with the position of the plate and maintains the fracture in place (Fig. 6).

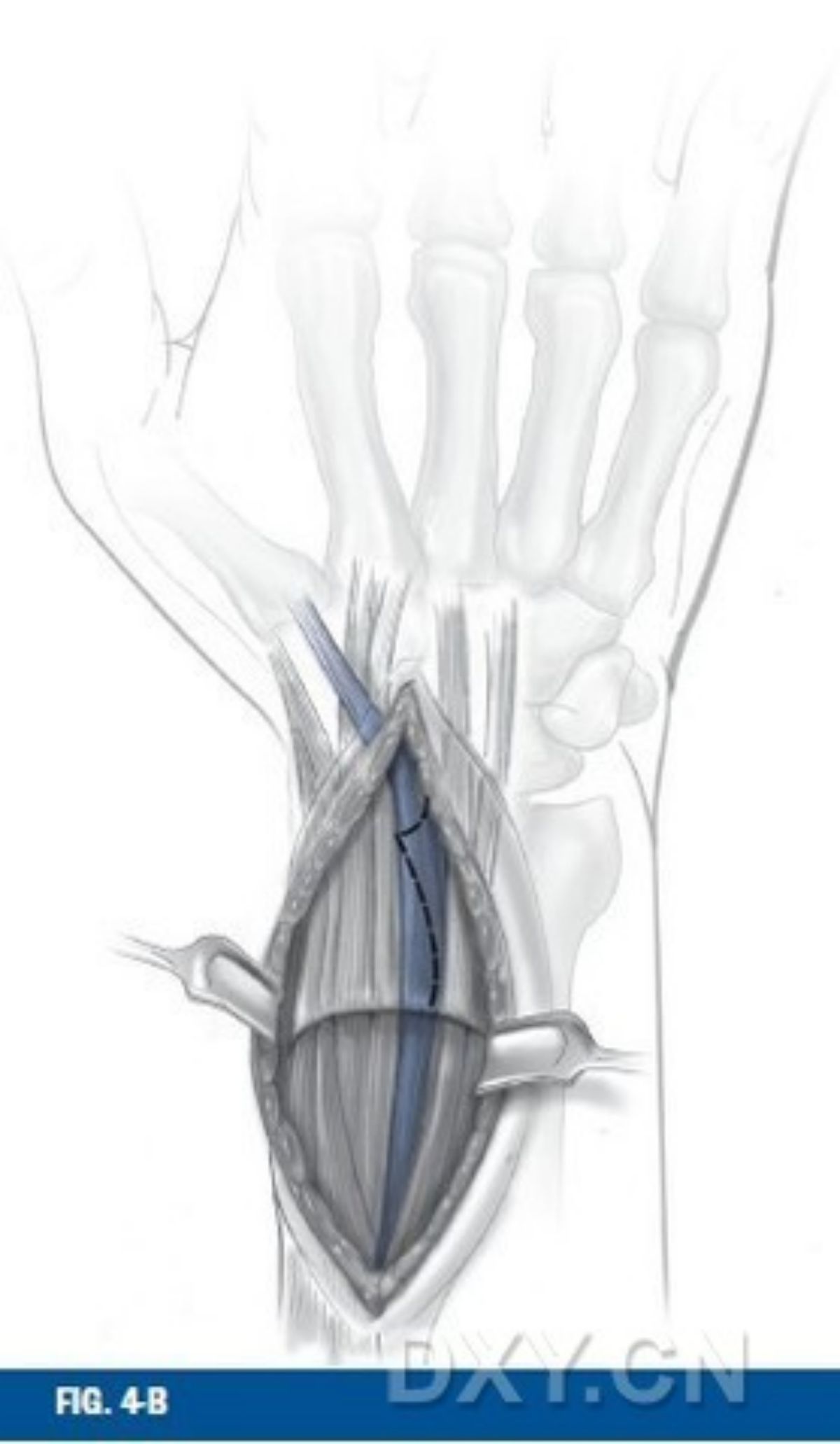
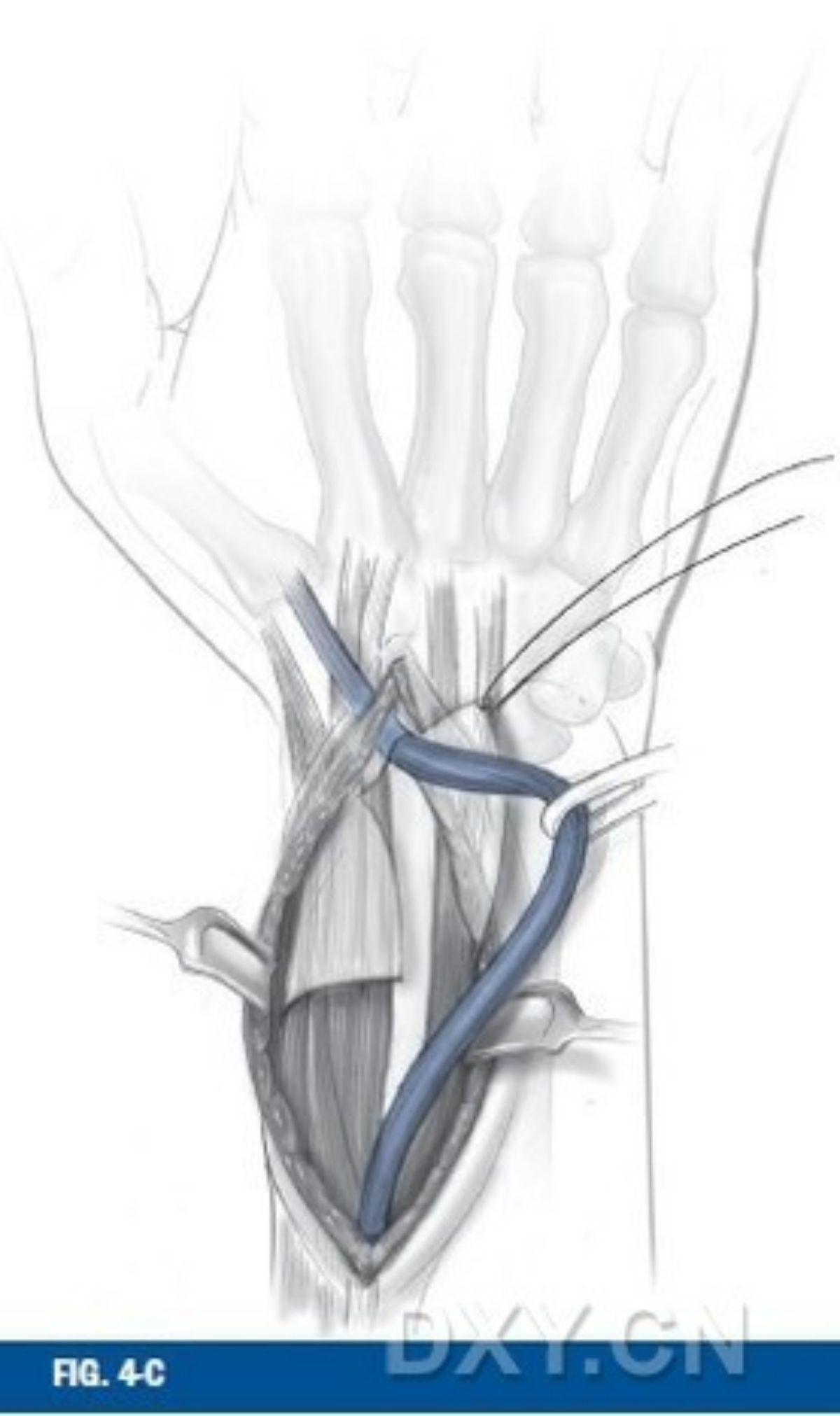
Fig. 4 Exposure of the dorsal surface of the distal radius. The support band is opened from the 3rd extensor interosseous compartment and the extensor hallucis longus tendon is retracted.

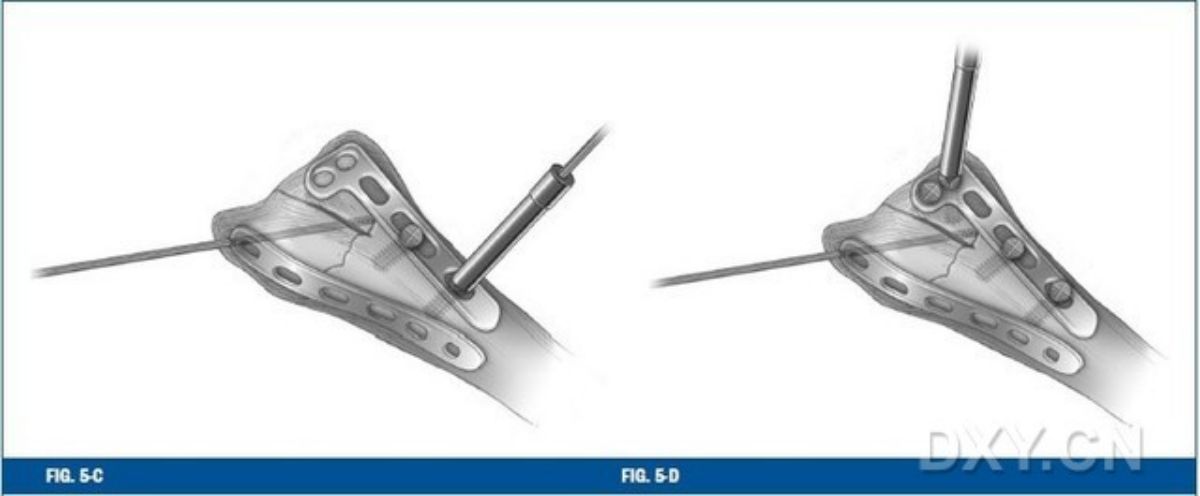
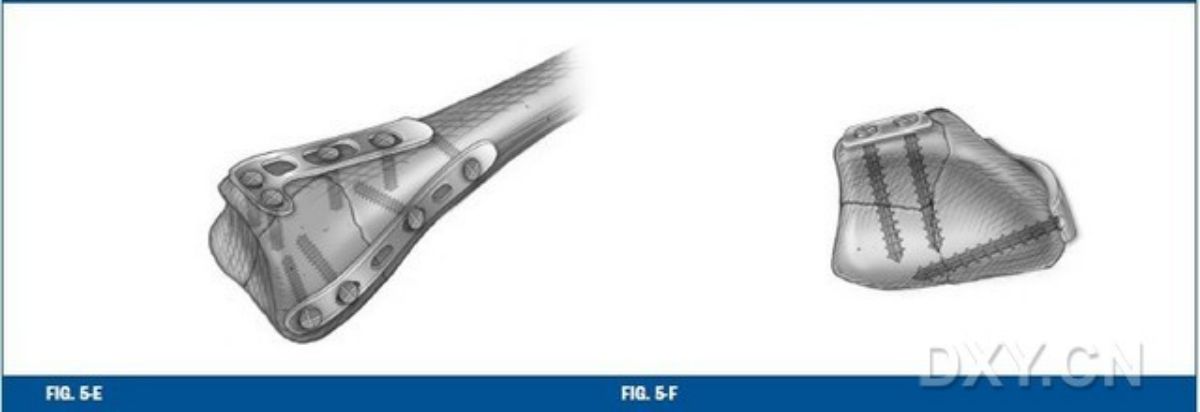
Fig. 5 For fixation of the dorsal aspect of the articular surface of the lunate, the dorsal "T" or "L" plate is usually shaped (Fig. 5-A and Fig. 5-B). Once the dorsal plate on the articular surface of the lunate has been secured, the radial column plate is secured (Figures 5-C through 5-F). The two plates are placed at an angle of 70 degrees to each other to improve the stability of the internal fixation.

Fig. 6 The radial column plate is properly shaped and placed in the radial column, noting the notch at the end of the plate, which allows the plate to avoid the temporary fixation of the Kirschner pin without interfering with the position of the plate.
Important concepts
Indications for Metacarpal Plate Fixation
Displaced metacarpal intra-articular fractures (Barton fractures)
displaced extra-articular fractures (Colles and Smith fractures). Stable fixation can be achieved with screw plates even in the presence of osteoporosis.
Displaced metacarpal lunate articular surface fractures
Indications for dorsal plate fixation
With intercarpal ligament injury
Displaced dorsal lunate joint surface fracture
Dorsally sheared radial carpal joint fracture dislocation
Contraindications to palmar plate fixation
Severe osteoporosis with significant functional limitations
Dorsal radial wrist fracture dislocation
Presence of multiple medical comorbidities
Contraindications to dorsal plate fixation
Multiple medical comorbidities
Non-displaced fractures
Mistakes easily made in palmar plate fixation
The position of the plate is very important because not only does the plate support the fracture mass, but proper positioning also prevents the distal locking screw from intruding into the radial carpal joint. Careful intraoperative radiographs, projected in the same direction as the radial inclination of the distal radius, allow for accurate visualisation of the articular surface of the radial side of the distal radius, which can also be more accurately visualised by placing the ulnar screws first during the operation.
Screw penetration of the dorsal cortex carries the risk of provoking the extensor tendon and causing tendon rupture. Locking screws perform differently from normal screws, and it is not necessary to penetrate the dorsal cortex with the screws.
Mistakes easily made with dorsal plate fixation
There is always a risk of screw penetration into the radial carpal joint, and similar to the approach described above in relation to the palmar plate, an oblique shot must be taken to determine if the screw position is secure.
If fixation of the radial column is performed first, the screws in the radial tuberosity will affect the evaluation of subsequent fixation of the articular surface resurfacing of the lunate.
Distal screws that are not screwed completely into the screw hole may agitate the tendon or even cause tendon rupture.
Post time: Dec-28-2023










